Female Cancer Diagnosis and Sexual Pain Dysfunction
For the latest installment in our Sex Plus Symposium series, the Kimberly Keiser and Associates team had the amazing opportunity to meet with a local expert in women’s sexual health-related disorders, Matthew A. Barker, MD.
Dr. Barker is a South Dakota native and returned home to teach and start a comprehensive pelvic floor center after finishing his fellowship. After graduating from the University of South Dakota Sanford School of Medicine, Dr. Barker went on to do a residency in Obstetrics & Gynecology at the University of Wisconsin in Madison, WI. He then did a fellowship in Female Pelvic Medicine and Reconstructive Surgery in Cincinnati, OH.
Dr. Barker is a Professor in the Departments of Obstetrics & Gynecology, Internal Medicine, and Neurosciences at the University of South Dakota Sanford School of Medicine. He is the Director of Female Pelvic Medicine and Reconstructive Surgery at Avera Health and practices urogynecology at Avera Medical Group Urogynecology. Dr. Barker was also recently elected to the Board of Directors for the American Urogynecologic Society.
In our session with Dr. Barker, he shared with us common issues with sexual function in patients with sexual pain disorders and following cancer treatments, understanding diagnosing and managing sexual dysfunction in women with sexual pain disorders and women who are cancer survivors, and how to approach treatment using a Sexual Medicine Program.
Studying Female Cancer Diagnosis and Treatment
According to a study done by Deborah Coady, it is estimated that one in three women will be diagnosed with cancer in her lifetime. There are more than 3 million women in the U.S. currently living with breast cancer — representing more than 40 percent of all women affected by cancer. Of those living with cancer, more than 64 percent of women’s cancer involves a sexual organ.
Patients with a history of gynecologic cancer have sexual dysfunction at some point in their cancer experience either before, during, or after treatment. These include things such as:
Vaginal dryness
Pain with intercourse
Loss of desire
Most gynecologic cancer survivors believe physicians should regularly ask about sexual issues, but more than half of the patients surveyed stated a physician never initiated the conversation during their care. Studies have shown that chances of surviving after or with ongoing therapy are now higher than ever.
“I appreciated Dr. Barker’s emphasis on the importance of interdisciplinary care, as many symptom presentations that physicians are met with are ones that have a connection to trauma and emotional wounds.”
Cancer Diagnosis and Emotional Well-Being
Coady’s study also stated that 15-30% of cancer patients will be diagnosed with depression and/or anxiety and approximately 79% of cancer patients are on medications for these issues.
In chronic illness, sexual health is a major determinant of how women rate their quality of life and is a reliable predictor of their overall emotional well-being. Sexual side effects may limit the acceptance or continuation of certain cancer treatments.
Sexual Health Communication
The treatment decision-making process should consider the impact on physical, sexual, and emotional function. The PLISSIT model is a sexuality assessment and intervention tool developed in the mid-1970s which follows these points:
Permission: Mention sexuality changes while also addressing cancer-related changes. This gives permission to think about the two together which legitimizes the topic.
Limited Information: Getting limited information about the sexual changes that can stem from treatment.
Specific Suggestion: A therapist makes specific suggestions that address sexual dysfunction.
Intensive Therapy: If needed, discuss more intensive therapy with your current mental health provider.
Sexual Function Affected by Sexual Pain
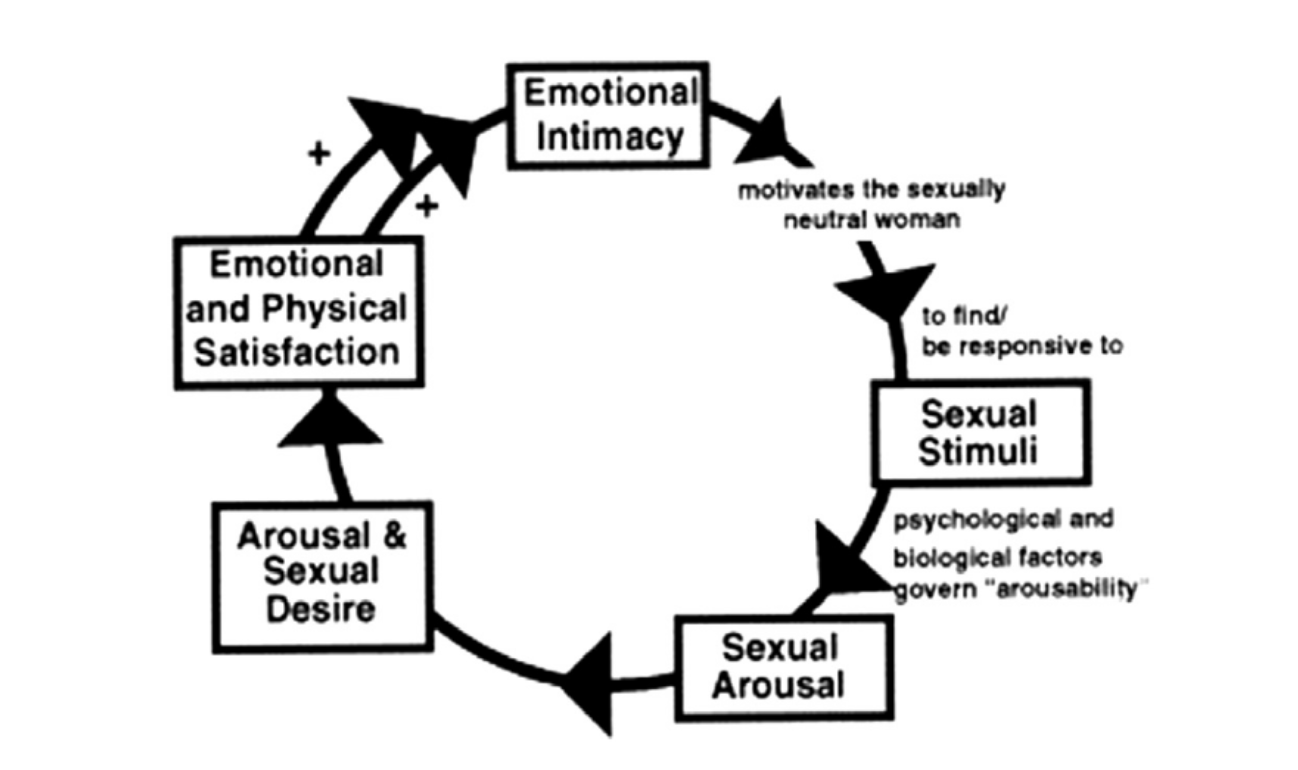
The sexual response cycle is a cyclical process as visualized above.** When sexual pain is present, this can lead to an avoidance of sexual activity altogether. Once there is pain, future encounters are met with a fear of that pain which can lead to partial avoidance of that sexual activity. This can then lead to sexual arousal disorder, orgasmic disorder, and a loss of sexual desire. Once those arise, this can lead to total avoidance of sexual activity and relationship difficulties.
Prevalence of Sexual Pain
In women treated for gynecologic cancer, the rate of sexual pain is as high as 55 percent of patients studied, with similar rates observed with rectal cancer treated with radiation therapy. Breast cancer survivors were reported with sexual pain in more than 45 percent of the patients studied.
Menopause
Another consideration for females experiencing sex therapy treatment is menopause. Menopause causes anatomical and physiological symptoms that impact sexual functioning.
The vasomotor symptom is commonly known as a hot flush — the sudden sensation of extreme heat in the upper body. A change in the hormonal and thermoregulatory mechanisms in turn leads to a hot flush. These can last up to five minutes and are characterized by perspiration, flushing, clamminess, anxiety, and heart palpitations. It may also interfere with sleep.
Vaginal symptoms include things such as vaginal or vulvar dryness, discharge, itching, and dyspareunia. The loss of superficial epithelial cells in the genitourinary tract causes thinning of the tissue. The loss of vaginal rugae and elasticity occurs with a narrowing and shortening of the vagina.
Genitourinary Syndrome of Menopause (GSM) is the constellation of symptoms and signs associated with decreased estrogen levels that can involve the genital system (vaginal or vulvar dryness, burning, dyspareunia) or the lower urinary tract (dysuria, urgency, frequency).
In part two of our session with Dr. Barker, we discuss tips and treatments for dealing with sexual pain and therapy.
*Stabile Transl Androl Urol 2015
**Basson Obstet Gynecol 2001